 Dr Åsa Jansson completed her PhD at the Centre for the History of the Emotions at Queen Mary University of London in 2014. Her thesis mapped the re-conceptualisation of melancholia as a modern biomedical mental disease in Victorian medicine.
Dr Åsa Jansson completed her PhD at the Centre for the History of the Emotions at Queen Mary University of London in 2014. Her thesis mapped the re-conceptualisation of melancholia as a modern biomedical mental disease in Victorian medicine.
In this blog post Åsa reviews the 51st volume in the series Wellcome Witnesses to Contemporary Medicine, which is devoted to the recent history of Seasonal Affective Disorder, or SAD.
C. Overy and E. M. Tansey (eds), The Recent History of Seasonal Affective Disorder (SAD). Wellcome Witnesses to Contemporary Medicine, vol. 51. London: Queen Mary, University of London, 2014. 132 pages. ISBN 978 0 90223 897 8
In 1976, South African psychiatrist Norman Rosenthal moved to New York with his family, where both he and his wife soon discovered that they were profoundly affected by the seasonal changes. During the dark winter months, they felt lethargic and suffered from low mood, but would begin to feel well again as the snow melted and the days got longer. When Rosenthal met Alfred Lewy at a party the two started talking about Lewy’s ongoing research on melatonin and the relationship between light and mood, and Rosenthal eventually joined Lewy’s research group at the National Institute of Health. The group was subsequently contacted by Herbert Kern, a man who had kept a detailed record of his seasonal mood changes. Kern himself believed that these changes were related to light exposure, and he became the first patient to be successfully treated with Rosenthal and Lewy’s experimental light therapy. The NIH research group proceeded to advertise in the Washington Post for people with seasonal mood changes, and received thousands of responses (Overy & Tansey, 2014: 9-17). In 1984, they published their research findings in a seminal article, ‘Seasonal affective disorder: A description of the syndrome and preliminary findings with light therapy’ (Rosenthal et al., 1984). SAD was born.

Image: Mental Health Support.
So begins the history of Seasonal Affective Disorder (SAD) as retold by the actors themselves and transcribed into the 51st volume of the Wellcome Trust witness seminar series. The current diagnostic status of SAD is contested, as is its targeted treatment, light therapy. One might argue that few people are oblivious to the emotional impact of seasonal changes, but the existence of the SAD diagnosis suggests an important difference between the ‘winter blues’ and a full-blown seasonal psychiatric disorder characterised by depressed mood, inertia, sleeplessness and over-eating. Moreover, these symptoms are believed to have a traceable biological aetiology. The diagnostic criteria for SAD are underpinned by three decades of research into the relationship between light, mood, and melatonin. Thus, the SAD experts participating in the witness seminar do not only claim that a distinct seasonally contingent depression exists, but that SAD is the first and as yet only psychiatric condition with defined and consistent biological markers. Judging by popular response to the advent of SAD, there is a significant population corresponding to the psychological and biological profile of this diagnostic category – people who suffer from debilitating depression during the darker months and whose symptoms are alleviated or even cured by daily exposure to bright light.
The Wellcome Witnesses to Contemporary Medicine Seminars are organised by Tilli Tansey’s History of Modern Biomedicine group, and constitute a space where participants in medical developments and events are invited to talk about their own memories of what happened. Since the first such meeting was held in 1993, the group have organised an impressive number of witness seminars on a wide range of topics, including heart transplant surgery, the medicalization of cannabis, and palliative care. Tansey describes the seminars as ‘a form of open peer review’, which provide ‘the opportunity to hear an array of voices, many little known, of individuals who were “there at the time” and thus able to question, ratify, or disagree with others’ accounts’ (quoted in Overy & Tansey, 2014: v). The seminars are transcribed, and participants are invited to add notes and clarifications to the transcripts, which are subsequently published. All volumes produced to date are freely available online. The witness seminar on SAD emerged through a collaboration between the History of Modern Biomedicine group and the Centre for the History of the Emotions, both presently located at Queen Mary, University of London. The seminar brings together several of the scientists and clinicians who were instrumental in the early development and reification of SAD; in addition to Rosenthal and Lewy most notably Josephine Arendt, a biologist who carried out pioneering research on melatonin and circadian rhythms in the 1980s. Other participants include prominent patient activists, such as Jennifer Eastwood, who founded the Seasonal Affective Disorder Organisation (SADA), a British patient organisation for SAD sufferers, as well as the organisaton’s current chair, Helen Hanson. The seminar was also attended by Tansey, as well as Thomas Dixon, Director of the Centre for the History of the Emotions.
Historians of the emotions and of psychiatry will no doubt find this witness seminar volume of particular interest. The seminar, held last year, was organised to coincide with the thirtieth anniversary of the first publication on SAD. SAD is, in other words, a young psychiatric disorder. This brief history makes it a particularly fascinating object of historical study. It is, in every sense of the word, a modern disorder created and reified through the interaction between clinicians, scientists, patients, funding bodies, insurance companies, policy makers, and the media. The SAD witness seminar sheds light on some of the key developments, particularly in the early years of the diagnosis. It also brings into focus a pertinent question that concerns most historians of medicine to a greater or lesser extent: ‘How do you create a belief in a real disorder that scientists and doctors and patients and the general public and journalists believe in and recognize and can all talk about?’ (Dixon, quoted in Overy & Tansey, 2014: 62). The evolution of a new medical concept is rarely a straightforward or inevitable development, but rather one that requires a significant amount of intellectual work. And, as illustrated by the SAD witness seminar, much also depends on chance and circumstances, on people being in a particular place at a particular time.
The seminar is preliminarily structured along three themes, outlined at the beginning of the transcript. The first of these aims to shed light on why the condition appeared and how it has changed over time, who was involved, and how the diagnosis has been received by the medical community. The second theme focuses on causation, that is, the perceived physiological basis of SAD, and the third addresses diagnostic criteria, treatment, and patient activism. The seminar starts off with Arendt offering a brief overview of scientific interest in mood, melatonin and circadian rhythms in the 1980s. Following her testimony, Rosenthal and Lewy talk about the early years of SAD research. Their stories form part of a detailed discussion about the science of circadian rhythms, light exposure, and mood changes. While the meeting as a whole loosely follows the prescribed format, the biological basis of SAD predominates. This should not deter readers from the humanities. On the contrary, this is partly what makes the SAD witness seminar such a valuable contribution to the history of psychiatry and of mood disorders in particular. What emerges is a biological history of a psychiatric condition that is contextual, limited, and (with the exception of a couple of brief references to seasonal depression in the works of Esquirol and Kraepelin) does not resort to ahistorical claims of universality by attempting to extend the research findings on seasonal mood changes into a past where SAD had not yet been invented. Moreover, the stories on offer are colourful and engaging, telling of a multitude of strategies and creative ideas that emerged through attempts to better understand why some people feel depressed during winter. What the testimonies from Rosenthal, Lewy, Arendt, and others illustrate more than anything is the human curiosity and desire to understand how things work that drive scientific research. Indeed, historians of early modern science will no doubt be pleased to find that the practice of self-experiment has not entirely gone out of fashion, with Lewy deciding to measure how his own melatonin levels changed when travelling through the time zones from Sydney to Washington (Overy & Tansey, 2014: 13-14).

‘Winter Light’ by Helen Hanson, artist and SADA chair (see also SAD at Thirty)
If the story of SAD in the laboratory is one of innovation and excitement, the story of how the diagnosis has been received in society at large is more chequered, but no less significant. The testimonies of Eastwood and other prominent patient activists in the UK provide an important perspective on the British situation. Unfortunately, however, no British clinicians were present at the seminar. Tansey states ‘on the record’ that this is not ‘for want of trying to find them, nor for inviting them’ (quoted in Overy & Tansey, 2014: 44). While this absence is regrettable, it is also informative. Eastwood and the other patient activists present speak of a reluctance of the National Health Service, as well as of British medical practitioners, to embrace the diagnosis or its targeted treatment. According to the narrative presented, the history of SAD in the UK has primarily been one of patient activism and (irregular) media attention.
Eastwood’s testimony of SAD in the UK highlights the relationship between the acceptance of a diagnosis and the presence of a marketable treatment, which largely makes up the final theme, but which also informs the seminar as a whole. According to Lewy, the ‘discovery’ of SAD was to a large extent facilitated by the simultaneous development of a successful treatment – light therapy. ‘Doctors don’t like feeling helpless and for them to be interested in a disorder they need to have a treatment’ (Lewy, quoted in Overy & Tansey, 2014: 12). Historians, particularly those concerned with the history of psychiatry, might beg to differ. It is no doubt the case that many psychiatric conditions have emerged and/or been popularised in correlation with the marketing of specific, predominantly pharmaceutical, treatments – what Healy (1999: 180) has termed ‘the Luke effect’.[1] However, psychiatrists have also paid significant attention to conditions perceived to be particularly difficult to treat – think, for instance, Borderline Personality Disorder prior to the advent and spread of Dialectical Behaviour Therapy. The interesting thing about SAD is that it belongs to neither of these categories. It is a disorder for which a clear and targeted treatment has existed more or less from the outset, but this has not been translated into widespread acceptance of the diagnosis by medical practitioners and mental health policy makers. The witness seminar discussion demonstrates that there exists a significant body of research on the role of melatonin and the sleep-wake cycle in seasonal depression. Yet despite existing evidence and patient testimonies on the efficacy of light therapy, national health services, funding bodies, and medical insurance companies have not been so quick to endorse this treatment. Most importantly perhaps, light therapy has negligible market value and is of little interest to pharmaceutical companies since, as Rosenthal poignantly remarks, ‘light is not a drug and not patentable’ (quoted in Overy & Tansey, 2014: 23).
The seminar participants emphasise that scientists are not in universal agreement over the precise mechanisms of light therapy, and that there is still much research to be done. Nevertheless, the comparatively advanced existing knowledge about the biological basis of SAD and the explicit and well-documented link between SAD as a diagnosis and light therapy as a targeted treatment makes this a highly unusual affective disorder. The question of biological markers for emotional illnesses has perturbed physicians since the emergence of psychiatric autopsies in early nineteenth-century asylum medicine. The practice of cutting into the brains of dead ‘lunatics’ often revealed tissue changes in patients suffering from severe, delusional forms of insanity, but in the case of emotional disorders, such as melancholia and moral insanity, visible lesions were usually absent. Physicians turned instead to the language of physiology to provide affective insanity with a biomedical foundation, but the search for quantifiable biological markers continued. In the seminar, SAD is referred to as the first successful case. Rosenthal remarks that it was once believed that ‘the so-called dexamethasone suppression test was the litmus test for depression, but it turned out to be non-specific’ (quoted in Overy & Tansey, 2014: 38). However, while the dexamethasone suppression test (DST) has not been widely incorporated into psychiatric diagnostics, the non-specificity Rosenthal refers to is strongly contested by many clinicians in the field, on the basis that there are two distinct illnesses that currently both fall under the banner of Major Depressive Episode. According to this view, the DST, which is used to measure production of the ‘stress hormone’ cortisol, is specific for what is referred to as melancholic or psychotic depression, or simply as melancholia (see e.g. Carroll, et al., 1981; Taylor & Fink, 2007; Shorter & Fink, 2010). This distinction between the ‘mainstream’ (non-psychotic) depression and a more severe type of mood disorder is not, however, recognised in the ‘psychiatric bible’, the American Psychiatric Association’s Diagnostic and Statistical Manual, despite attempts to have ‘melancholia’ instated as a separate diagnosis in DSM-5.
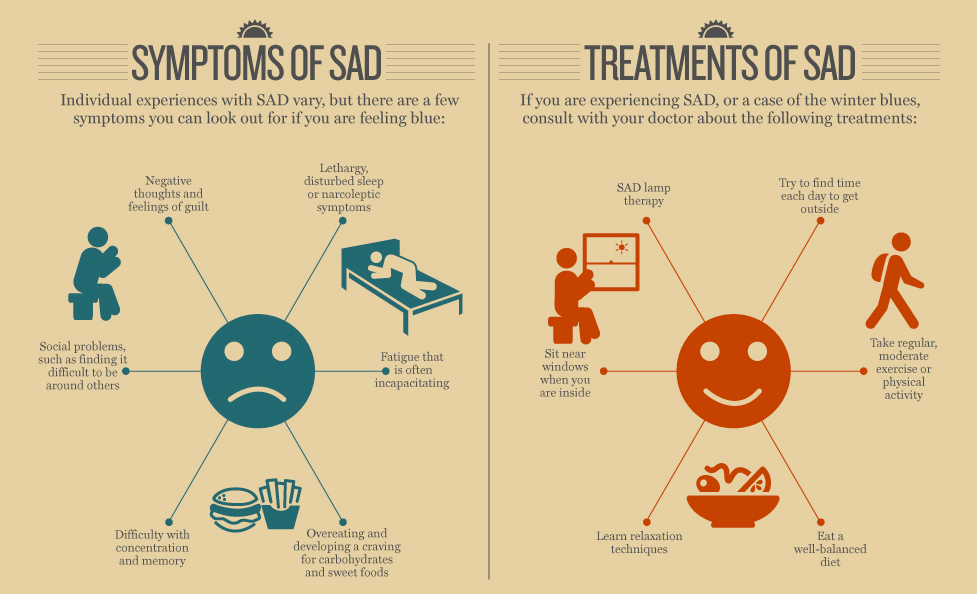
Infographic from Access Healthcare Services.
This comparison between SAD and melancholic depression is symbolic of the ambivalence of diagnostic criteria and boundaries. The history of diagnostic practices in psychiatry is characterised by a constant re-drawing of categories, prompted at least as much by epistemological trends, fraternal relationships, market forces, and wider cultural norms as by new empirical evidence. Thus, the seminar transcript does not only constitute a fascinating and much-needed contribution to the history of the biological basis of disordered affectivity, it also helps shed light on a topic of much significance for clinicians and historians alike: the politics of diagnosis. Classification has been a topic of heated debate throughout the history of the psychiatric profession, and remains so today, as evidenced by reactions to the publication of DSM-5 in 2013 (see for instance the series of ‘Responses to DSM-5’ in the British Medical Journal). The SAD witness seminar transcript offers a snapshot of the relationship between psychiatry, the market, policy concerns, and patient advocacy. With the exception of a brief statement by Dixon (Overy & Tansey, 2014: 62-63), what the witness seminar format does not do is explicitly address the historical contingency of psychiatric diagnoses, or offer critical reflections on the narrative(s) presented. The question arises, then, whether the SAD volume should be approached as a history of this disorder, or whether it should be treated primarily as raw source material for scholars interested in the history of mood disorders. Tansey suggests that ‘the point of these meetings is not to hear from historians like Thomas and me but to hear from you, the authentic voices’ (quoted in Overy & Tansey, 2014: 4). This prompts a question that underpins the witness seminar format, and upon which there is much disagreement both within and outside of historical scholarship: can we ever recover ‘what really happened’?
Notwithstanding Tansey’s remark, the role of historians in the SAD seminar, and in the witness seminar format more generally, is ambivalent. Tansey and Dixon are not merely passive observers; moreover, the seminar would not have occurred in the first place had they not taken an interest in SAD, organised the meeting, and decided who to invite. At the same time, they do not intervene into the storylines offered by the other participants, the ‘authentic voices’. Would a more active participation of historians in the SAD witness seminar have resulted in a more ‘complete’ history? It would undoubtedly have produced a different kind of history, but there is a risk that the ‘snapshot’ testimonies and some of the valuable scientific detail would be lost. Moreover, historians are no more capable of ‘objective’ history than the subjects they study (though some might like to think so!). An historian’s ‘observer’ perspective on SAD would be as partial and subjective as the testimonies of historical actors. This is precisely why the witness seminars form such an invaluable contribution to the history of medicine. We need as many different partial perspectives as possible; this is where the real ‘promise of objectivity’ lies (Haraway, 1988: 586). What the SAD story illustrates above all is the pressing need for closer interaction – in any format – between clinicians, patients, and historians of medicine, particularly where psychiatry is concerned. Psychological distress is one of the greatest public (and individual) health challenges of our time, yet mental health services remain disastrously under-funded, and treatment approaches are perilously reliant upon on the interests of drug manufacturers. In this climate, a more flexible and dynamic approach to psychiatric illness is urgently needed, one that will allow each individual who experiences psychological distress to receive the best possible support, whether that takes the form of medication, community activities, counselling, or very bright light. Because, as Dixon suggests during the seminar, what the history of SAD is really about is ‘real human beings having real suffering and frustrations of trying to create knowledge and treatment around that’ (p. 62).
Download the full transcript of the SAD Witness Seminar
Listen to Natlalie Steed’s specially commissioned podcast ‘SAD at Thirty’
Watch video clips of Norman Rosenthal talking about SAD
Read an interview with Norman Rosenthal by Jules Evans
Read more from Åsa Jansson about melancholia and problems of retrospective diagnosis
Notes:
[1] Healy derives the term from the Parable of the Sower in the Gospel of Luke, in which the sower scatters seeds that fall on the path, on the rocks, among the thorns, and on fertile soil (respectively). Only the latter yield a good crop, the lesson from which is that bountiful crops will come to those who listen and retain what they hear, which, Healy argues, ‘drug companies do very successfully.’
Bibliography:
Carroll, BJ et al. (1981) A specific laboratory test for the diagnosis of melancholia. Standardization, validation and clinical utility. Archives of General Psychiatry (38)1: 15-22.
Haraway, D (1988) Situated knowledges: The science question in feminism and the privilege of partial perspective. Feminist Theory (14)3: 575-599.
Healy, D (1997) The Antidepressant Era. Cambridge, Massachusetts: Harvard University Press.
Rosenthal NE et al. (1984) Seasonal affective disorder: A description of the syndrome and preliminary findings with light therapy. Archives of General Psychiatry (41)1: 72–80.
Shorter E and Fink M (2010) Endocrine Psychiatry: Solving the Riddle of Melancholia. Oxford: Oxford University Press.
Taylor MA and Fink M (2007) Resurrecting melancholia. Acta Psychiatrica Scandinavica (115) Supplement 433: 14-20.

