This is a guest post by Chris Millard. Chris is a lecturer in history at the University of Sheffield, and has just completed his Wellcome Trust-funded postdoctoral research at QMUL with interests in the histories of psychological categories, the welfare state, the emotions and the idea of ‘parity of esteem for mental heath’. His book, A History of Self-Harm in Britain, was published (open access) by Palgrave Macmillan in 2015.
This is a guest post by Chris Millard. Chris is a lecturer in history at the University of Sheffield, and has just completed his Wellcome Trust-funded postdoctoral research at QMUL with interests in the histories of psychological categories, the welfare state, the emotions and the idea of ‘parity of esteem for mental heath’. His book, A History of Self-Harm in Britain, was published (open access) by Palgrave Macmillan in 2015.
A few months ago, I spoke at one of the Centre for the History of the Emotions’ lunchtime seminars on the subject of my current research – a rare form of child abuse that used to be called Munchausen Syndrome by Proxy. It is now known by the rather more descriptive moniker of Fabricated or Induced Illness by Proxy (FII by proxy). As the name suggests, it describes child abuse where a carer (overwhelmingly Mothers in the medical literature) either fakes or causes illness in those under their care.
A recent conviction for child abuse and welfare fraud has been in the news, making it timely to revisit the topic. In that particular case, Munchausen / FII by proxy is not mentioned. However the case involves systematic faking of illness in two children by a mother who, according to the police ‘lied at every opportunity, presenting herself as a lone parent coping with ill and vulnerable children.’
Throughout this blog, I will use the terms Munchausen Syndrome by Proxy and MSbP because these were the terms in general use at the time (1970s-2000s). The term was proposed in 1977 by Leeds-based peadiatrician S.R. (Roy) Meadow, who described two long-running cases. In the first a 6-year-old girl had blood added to her urine samples, provoking increasingly invasive diagnostic procedures. In the second a 6-month-old infant was eventually killed by the covert administration of salt, which caused him to ‘fail to thrive’.
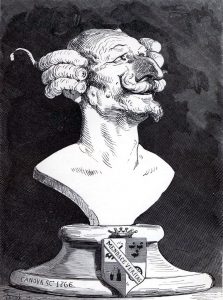
Meadow used the term ‘Munchausen’ in relation to these cases in homage to Richard Asher. Asher, a London heamatologist and polymath (and Father to Jane Asher), invoked the fictionalised figure of 19th-century raconteur Baron Munchausen in 1951 to describe patients who repeatedly presented at hospital, pretending to be ill. For both Asher and Meadow it was the long-running saga of these deceptions that made the Munchausen term seem apt.
My point of entry into the tangled web of MSbP was a controversial set of convictions for child murder in the 1990s and early 2000s. The overturning of these convictions proved the undoing of Meadow, whose expert testimony had helped to secure the ‘guilty’ verdicts. Sally Clark, Angela Cannings, Trupti Patel and Donna Anthony were all accused of murdering their children, in cases previously categorized as Sudden Infant Death Syndrome (SIDS) – known colloquially as ‘cot death’. Meadow argued instead that these women had murdered their children for attention, and badly misused statistics in the process.
Meadow was struck off the medical register from gross misconduct in the aftermath of the successful appeals. Although he was later reinstated, he retired and went into near seclusion. My paper attempted to offer a new perspective on how this diagnosis of MSbP could have blown up so spectacularly in his face.
I tried to shy away from the explanations that emphasized Meadow’s misogyny and desire to persecute women. At the time of his case for misconduct with the General Medical Council, his sexuality was called into question in the press (as if it were relevant); his participation in an amateur dramatic production of Arthur Miller’s The Crucible (as the Witchfinder General) was also dredged up from his past. Blaming individuals and their real or imagined foibles and motivations is undoubtedly part of the story, but on its own is historically unsatisfying. Human beings make choices and act in certain ways whilst deeply imbedded in cultural assumptions and historically specific ‘common sense’. I sought a more structural backdrop to this controversy.
I came up with an historical comparison – looking at cases labeled MSbP during the first few years after 1977, and then those in the late 1990s (which led to convictions for child-murder). Two distinct pictures emerged. In the first set of cases, mothers presented children over and over again, sometimes for months and years before foul play was suspected. Huge amounts of evidence was collected that made no medical sense: foul, bloody urine samples were collected from one patient, with clear samples an hour or so either side. A child would relapse into a coma after a week of steady improvement; the child would improve again, only to become comatose once more, extraordinarily suddenly. In these cases extensive surveillance and monitoring was carried out, by nurses, and then, later in the 1980s, by covert video recording. MSbP was an eventual answer to make sense of an enormous amount of conflicting medical evidence. Sometimes exceptionally high-tech methods were used. A baby’s blood was marked with mildly radioactive substances to ascertain the bleeding point in its mouth – none was found. However, the blood around the infant’s mouth at the next episode contained no more than background radiation, and matched the mother’s blood type when tested. This was a long saga of cat-and-mouse, carried out in hospitals, under extreme levels of surveillance.
By contrast, the court cases of the 1990s/2000s were based upon infant mortality statistics for SIDS/cot death. SIDS is a blanket term used to refer to all sudden deaths with no discernible cause. In Sally Clark’s case, after her second son died suddenly she became a suspect for child murder. This was based on the supposed statistical improbability for two or more SIDS deaths in the same affluent, non-smoking family. This underwrote the infamous Meadow’s Law: ‘one sudden infant death is a tragedy, two is suspicious and three is murder, unless proved otherwise’. These cases were thus rooted in statistical reasoning and infant mortality calculations.
Thus it isn’t that Meadow got somehow ‘carried away’ with statistics, but that the whole basis for MSbP had changed. From a smorgasbord of conflicting medical evidence, over a long period and under tight surveillance, we can see a shift to a simplistic kind of statistical reasoning. This reasoning functioned as a sort of ‘pinch point’ or pivot: get this wrong and everything tumbles.
Whilst these objects – the hospital-based and statistically-based diagnoses – were connected by naming them both ‘Munchausen Syndrome by Proxy’, they were otherwise vastly dissimilar. In its migration from the hospital ward to the courtroom (via the Registrar General’s office for the statistics) – MSbP became a precarious allegation with a single point of failure. Context matters, and history is well-placed to provide it.