Pain is a sensation – and a topic – that has recently attracted much attention among historians, particularly those working in the field of the history of emotions. This post interrogates perceptions of mental pain that link this feeling to suicidality, by tracing some of the historical roots of an assumption that is often taken for granted in the present.
‘What hurts more? Physical or mental pain?’ According to a 2008 study investigating the difference between the two, subjects found mental pain more difficult to cope with, mainly because of its lingering quality. Physical pain, once gone, could be forgotten, the study concluded, whereas humans are more likely to relive experiences of psychological pain, and find such memories to be more vivid and more painful.
The same question was asked in an online forum the following year, with respondents overwhelmingly declaring mental pain to be the worst of the two. One contributor succinctly explained: ‘Physical u can get over… Mental sticks with u for forever and ever…. Breaks ups, deaths, abuse stuff tht will stick with u until u die….’. Others agreed, with one poster asserting that ‘I have been beat by cops and prison goon squads but nothing hurt as bad as being used and having my heart broke.’ The same question was posed again, in the same forum, two years later, with much the same result. ‘I had a fair shot of mental pain back a while back with a fair few things’, wrote one participant, ‘and i would of rather been fighting Mike Tyson than thinking that way’. Response upon response reaffirmed this view. Most people, it seemed, would far rather endure physical than psychological pain. Why? As one of the respondents, Dagon, explained, ‘Physical pain comes in many forms and can be fixed, Mental pain comes from the imagination and it can affect ones health, create depression, drive one to suicide, cause abberrations in ones thinking, and cause insanity.’
The belief that mental pain can be a sign of madness, and that it causes individuals to become suicidal has long been a focus of psychiatric inquiries into the emotional life of humans. In the early 1990s, British psychiatrist Edwin Schneidman claimed that suicide was caused by ‘psychache’, a term he used to describe ‘intolerable psychological pain.’ His work has since formed the basis for further research into this topic. Apparently unbeknownst to Schneidman, however, his words echoed those of a nineteenth-century German psychiatrist who suggested in 1874 that melancholia, a form of affective insanity, was characterised by a mental pain that often led sufferers to become suicidal. Richard von Krafft-Ebing described this psychic pain as analogous to the neuralgia of the spinal cord and lower brain – a ‘psychic neuralgia’, or ‘psychalgia’.
In Krafft-Ebing’s view, severe emotional pain was pathological when it arose internally, without adequate cause and as the result of a morbid physiological reaction, usually brought about through repeated ‘irritation’ of the brain. For sufferers it would appear as if the world around them had changed, they would feel trapped in this painful emotional state, powerless to resist the despair that engulfed them. Eventually, a single solution would appear as the only possible escape: suicide. The pain was often so unbearable, Krafft-Ebing argued, that melancholics must be watched over at all times in order to prevent such individuals from taking their own life. ‘The shrewdness and persistence of such sick people in the pursuit of their suicidal intentions are often extraordinary’, he warned, so much so that even ‘[t]he straitjacket is thus no guarantee against suicide.’
The view that melancholics were prone to suicidal tendencies due the unbearable mental pain that characterised the condition was pervasive also among British physicians in the last quarter of the nineteenth century. However, only a few decades earlier medical literature on melancholia contained few references to ‘suicidal’ tendencies, and even fewer to ‘mental pain’. The latter was a relatively late addition to the vocabulary of nineteenth-century psychiatry (or psychological medicine, as it was usually referred to in Britain at the time). Its usage as an analogy to physical pain emerged in part through the appropriation of language from experimental physiology to speak about mental phenomena. Within a new scientific framework where emotions were explained as automated physiological reactions, mental pain was a sensation caused by disordered brain activity. However, the term has a longer and multifaceted history – in the early modern period, before it gained popularity in internal medicine, ‘mental pain’ had strong religious connotations, expressing a suffering experienced in response to having sinned against God. This was primarily the way nineteenth-century melancholic patients themselves explained their emotional suffering – as a torturous pain divinely inflicted in response to having committed ‘the unpardonable sin’. This spiritual early modern conception of mental pain was translated by Victorian physicians onto the pages of asylum casebooks as ‘religious delusions’ brought on by the cerebral disorder of melancholia.
‘Suicidal’, conversely, was born into medical language as a practical term with legal implications. As a result of early nineteenth-century lunacy law reform culminating in the 1845 Lunacy Acts, when patients arrived into the Victorian asylum they did so accompanied by a medical certificate of insanity and a reception order, which asked the certifying authority to state (largely for reasons of safety) whether the lunatic was ‘epileptic’, ‘suicidal’, or ‘dangerous to others’. This information was transferred to the asylum casebook, where a diagnosis would be entered alongside it. Such information would then be brought together into neat tables, tallied up, and reported to the Lunacy Commission on an annual basis. Year after year, such statistical tables indicated that of all suicidal lunatics, the vast majority were melancholics, and of all melancholics, the majority were suicidal.
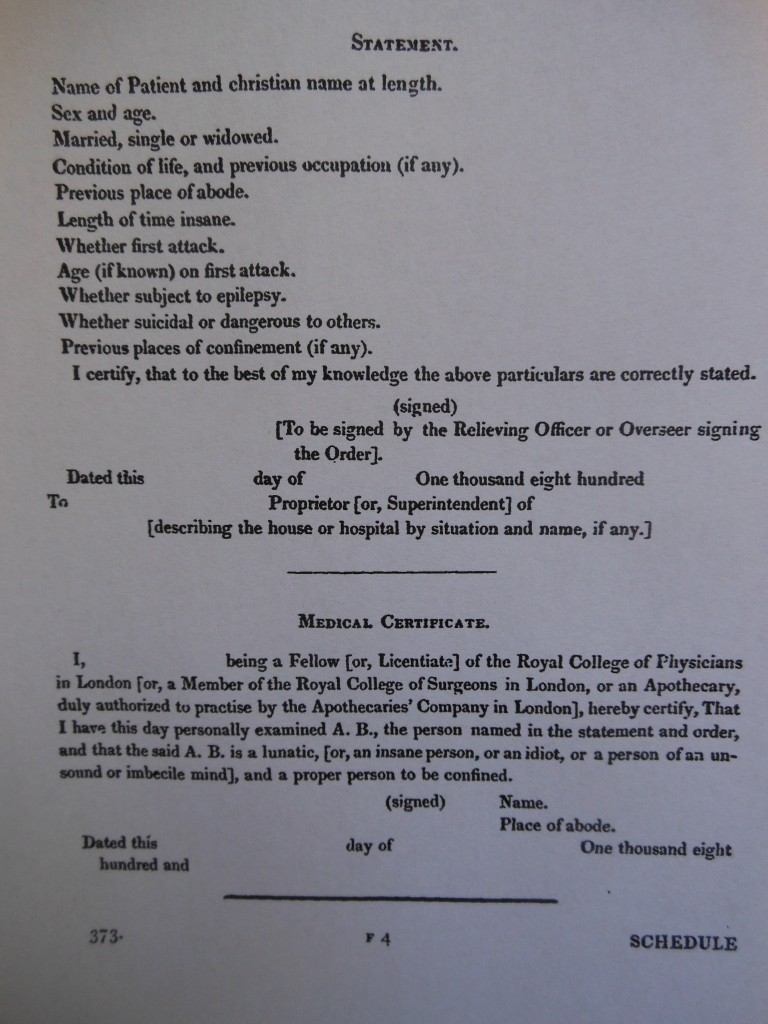
Template for a medical certificate of insanity, provided as an appendix to the 1845 Care and Treatment of Lunatics Act.
Historians have concluded that due to the way it was deployed, ‘suicidal’ was semantically ambivalent, a conundrum also noted by Victorian physicians themselves. The term was believed to be applied to a range of different acts and expressions, and while statistical reports suggested that a large number of asylums patients were suicidal, remarkably few suicides occurred in the asylum. Thus, both nineteenth-century physicians and twentieth- and twenty-first century historians have suggested that the term ‘suicidal’ was misleading, arguing that only a small number of those who received the label upon certification were in fact ‘actively’ suicidal.
However, the practices that created the medical concept ‘suicidal’ and wedded it to melancholia and mental pain did not generate incorrect information, they produced context-specific knowledge that had, just like other kinds of medico-scientific knowledge, an internal logic. The creation of ‘suicidal’ as a category on medical certificates generated numerical data on the suicidality of asylum patients, data that was recorded together with a diagnosis. Such information was merged into statistical tables and supplied to the Lunacy Commission on a yearly basis, and enabled physicians to argue that melancholics were by far the most ‘suicidal’ of all lunatics. At the same time, melancholic patients expressed a profound spiritual pain and suffering, translated by their doctors as an intolerable mental pain that was a psychological manifestation of a disordered neurological process. This pain was assigned as the chief cause of the overwhelming suicidality that asylum statistics suggested to be a typical feature of melancholia.The relationship between melancholia, mental pain, and suicidality eventually became self-perpetuating and circular, as illustrated by the following warning issued by a famous Victorian physician: ‘Suicidal feelings and attempts are common in melancholia, so much so that one suspects their actual or possible existence even when they have not been openly manifested.’
In twenty-first century psy-literature, the close relationship between mental pain and suicidality is equally taken for granted – intolerable mental pain produces suicidal thoughts and gestures, which sometimes lead to suicide. While such similarities across time and space could be perceived as speaking to a universal, timeless nature of this assumption, a closer look at its roots suggests a more complex picture. The belief that profound mental pain leads human beings to become suicidal is neither self-evident nor inevitable – it emerged as medical knowledge through the intersecting of spiritual beliefs, physiological language, and statistical practices.

Great & informative read, thank you. After spending 36 years with my mum who we were told was manic depressive I believe wholeheartedly that mental illness is completely delapitating & torturous. She suffered immensely with bi polar. She was a strong woman & a force to be reckoned with when she was ‘good’ so when she ‘wasn’t good’ she saw herself in very harsh lights which resulted in fast & sometimes furious, sometimes frustrating but always devastating spirals. More frequent &much worse as time went on. On meds, off meds, self medicating. Her journey ended with her devastating decision to take matters into her own hands & she ended her, almost lifelong battle,at age 72. I am so thankful that this topic is being researched in greater depth, perhaps those suffering with mental anguish & depression will have more assistance & understanding as a result. Thank you.
Pingback: Love, Pain, Ecstasy, and Murder: An Emotional Christmas | The History of Emotions Blog