This guest post by Evelien Lemmens is part of Gut Feelings Week, in which a group of scholars participating in the conference Gut Feeling: Digestive Health in Nineteenth-Century Culture explore different aspects of digestion.
Evelien Lemmens is a PhD candidate researching the relationship between diet, digestion and emotional health in Britain between 1850 and 1937. She is part of the Wellcome Trust funded ‘Living with Feeling’ project at Queen Mary University of London’s Centre for the History of Emotions. Her research interests include history of emotions, social history of medicine, and gender history.
How do you solve a problem like dyspepsia?
Dyspepsia, as a term used in lay literature and endorsed by the non-medical community, experienced its glory days during the nineteenth century. Gaining traction from around 1800 onwards, the term’s use was spurred on by the growth of the British press, significant attention to the ailment by manufacturers of patent medicine, and an increased demand for public education on topics of diet, cooking, and domestic science. By the 1880s, self-proclaimed “dyspeptics” were found, as per the physician Thomas Clifford Allbutt and fellow commentators, on every street-corner and formed a real nuisance for the medical community. However, throughout its rise and fall, and up until today, the term ‘dyspepsia’ remains a vague and flexible term.
Early example of a published monograph showing ‘dyspepy’ on its title page. James Rymer, A Treatise Upon Indigestion, and the Hypochondriac Disease, 5th edn (London, 1789).
Dyspepsia (as dyſpepſy) first made an appearance in an English-language publication in 1661, but it was not until the 1780s that it appeared in the title of one. Originally limited to use in medical and academic texts, ideas of dyspepsia steadily infiltrated lay literature, gaining increased momentum from 1800 onwards. This increased awareness resulted in a wider cultural attention for and appropriation of dyspepsia. During the first half of the nineteenth century, dyspepsia transformed from a disorder of the intellectual elite to the national disease of Britain and America. This was allowed for by a broadening of dyspepsia’s aetiology, which came to comprise every possible cause: mental overwork; emotional agitation; poor ventilation; substandard food quality and preparation; improper dietary habits and lifestyle; tightly-laced corsets; poor oral hygiene and so on. The breadth of dyspepsia’s aetiology meant that anyone could fall victim to it, and it became a perfect disorder for ‘cure-all’ patent medicines to target.
Despite its prevalence in publications, especially during the second half of the nineteenth century, dyspepsia has remained a difficult ailment to grasp. By its most basic definition, dyspepsia equates to indigestion. However, the term’s meaning increased in breadth and complexity at the start of the nineteenth century, and the surge in attempts to delineate dyspepsia resulted in a critical blurring of the ailment entailed.
This blurring of dyspepsia contributed to divergent judgements of the ailment. On the one hand, dyspepsia could be accepted as an objective and legitimate category of diagnosis, as it was used in official medical reports, court cases, and parliamentary records. Dyspepsia could alter how an individual’s actions were judged, especially if these were considered erratic or out of character. For example, an 1894 inquest into the suicide of Captain Charles Ernest Cureton – an occasion of “considerable gloom” – offers a verdict of “suicide while temporarily insane” resulting from his dyspepsia, hypochondria, and depression “in spirits.” Here, dyspepsia connotes more than a failing of digestion.
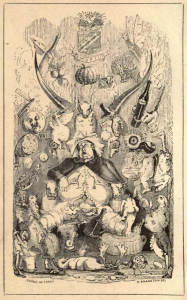
Frontispiece of Sydney Whiting’s Memoirs of a Stomach, showing a man suffering from dyspepsia and indigestion resulting from over-indulgence and faulty habits.
On the other hand, dyspepsia was often depicted as a woolly excuse of a condition, amounting to little more than indigestion following one’s own faulty eating habits, accompanied with unwarranted self-pity. These “martyrs to dyspepsia” became a favourite target of satire in periodicals like Fun and Judy, and fear inciting advertisements for dyspepsia remedies, which presented the ailment as life-wrecking, were criticised as “puffery.” The social acceptance of dyspepsia was dependent on the interpretation of the term, and fluctuated over time, genre, class, and gender.
Today’s dictionaries continue to exemplify this difficulty, as is demonstrated by definitions of dyspepsia in the Oxford Concise Medical Dictionary and the Oxford English Dictionary. The CMD, a standard reference guide for medical practitioners, defines dyspepsia as:
(indigestion) n. disordered digestion: usually applied to pain or discomfort in the lower chest or upper abdomen after eating and sometimes accompanied by nausea, vomiting, or a feeling of unease or fullness after eating.
Meanwhile the OED, the accepted authority on the English language, defines dyspepsia as:
Difficulty or derangement of digestion; indigestion: applied to various forms of disorder of the digestive organs, esp. the stomach, usually involving weakness, loss of appetite, and depression of spirits.
While both present dyspepsia as disordered digestion, the CMD mentions nothing of the accompanying mental and emotional dimensions that are present in the OED. Furthermore, while the CMD focuses very much on symptoms post-eating, the OED highlights a loss of appetite. The difference is striking: a sufferer of dyspepsia in the OED is inflicted with weakness and poor emotional health, as well as a lack of interest in food, whereas the sufferer in the CMD predominantly has digestive complaints following the intake of food.
Similarly, dyspepsia is still included in the International Statistical Classification of Diseases and Related Health Problems (ICD-10) today. However, the diagnosis of dyspepsia is splintered and occurs in a myriad of diagnostic categories: a disease of the digestive system (K30); symptoms and signs involving the digestive system and abdomen (R10-19); or somatoform disorders of nonpsychotic mental, behavioural of neurodevelopmental symptoms (F45.8).
This splintered and dynamic nature of medical diagnoses, past and present, highlights the value of medical anthropology in studying the cultural and social history of medicine and health. In The Body Multiple, Annemarie Mol presents an ethnography of the day-to-day diagnosis and treatment of atherosclerosis, a comparatively straightforward ailment. Following “objects while they are enacted in practice,” which she terms praxiography, she notes the significant discrepancies between different specialisms (surgeons, physicians, internists, radiologists, pathologists) in diagnosing, explaining, and treating atherosclerosis. Though these discrepancies complement each other and can work together, they offer different interpretations of the disease and require tools of translation between them. In this study, Mol clearly demonstrates that medicine “has gaps and tensions inside it. It hangs together, but not quite as a whole.” Her approach – tracing the enactment of pathology – offers a new way for historians to approach the history of medicine through practice theory, which will illuminate dynamic tensions within and between historical ailments.
Follow the conference using the hashtag #GutFeelings
